A Multi-Technology Playbook for Optimizing Osseointegration, Mechanical Integrity, and Cost-Effectiveness
Executive Summary
Laser Powder Bed Fusion (L-PBF) has undeniably revolutionized the design and manufacture of orthopaedic implants, particularly those featuring complex, integral porous structures for biological fixation.1 This advancement has unlocked new possibilities in patient-specific devices and sophisticated lattice designs. However, this progress prompts a critical engineering question: for implants where bulk mechanical strength, fatigue life, and ductility are paramount—such as in high-load joint arthroplasty or trauma applications—is a fully porous, additively manufactured (AM) structure the optimal design when only the surface requires porosity for osseointegration? The fundamental material science suggests a trade-off that cannot be ignored.
This white paper presents the definitive engineering solution: a “surface-centric” paradigm that decouples bulk material properties from surface characteristics. Croom Medical’s vertically integrated, multi-technology platform enables the intelligent combination of high-strength substrates—produced via established methods like forging and machining—with application-specific surface modifications, including additive coatings and subtractive etching. This approach delivers implant solutions that optimize the critical bio-mechanical balance, achieving superior clinical performance, enhanced cost-effectiveness, and greater design freedom.
Our methodology is built on three core engineering value propositions:
- Optimized Bio-Mechanical Performance: By starting with a wrought or forged substrate, we harness superior, isotropic mechanical properties, including higher fatigue strength and ductility, which are critical for long-term implant survivorship.3 This robust core is then augmented with a surface engineered specifically for predictable and effective osseointegration, creating an implant that does not compromise on either mechanical integrity or biological response.5
- Application-Specific Solutions: We reject a “one-size-fits-all” manufacturing approach. Instead, we select the ideal technology for the specific clinical challenge. This could be a Titanium Plasma Spray (TPS) coating on a forged Cobalt-Chrome (CoCr) femoral stem, a uniform acid-etched surface on a precision-machined Ti-6Al-4V trauma plate, or a hybrid construct combining AM, machining, and coating for a next-generation acetabular cup.7 This ensures the most efficient and effective solution for each unique application.
- Expanded Design Freedom and Material Portfolio: Our multi-technology platform enables the application of proven porous surfaces to a wider range of materials not readily suited for L-PBF, including high-fatigue CoCr alloys and advanced polymers like PEEK.10 This expands the toolkit available to R&D engineers, allowing for greater innovation and optimization across an OEM’s entire product portfolio.
Croom Medical operates as a technology-agnostic partner, guiding our clients from initial concept through to final, validated production under a single, integrated ISO 13485 quality management system.
Schedule a technical consultation with our materials science and surface engineering team to co-engineer the optimal surface for your next implant project.
2. Introduction: Re-evaluating the Porous Implant Paradigm
The advent of additive manufacturing has bifurcated the approach to creating porous orthopaedic implants, leading to two distinct engineering philosophies. Understanding the fundamental trade-offs between these paradigms is essential for optimizing implant design, performance, and commercial viability.
2.1 The Engineering Dichotomy: AM-Centric vs. Surface-Centric Porosity
The AM-centric paradigm leverages technologies like Laser Powder Bed Fusion (L-PBF) to fabricate monolithic implants where the porous architecture is an integral part of the entire structure. This approach offers unparalleled geometric freedom, enabling the creation of complex internal lattices designed to mimic the modulus of bone, thereby reducing stress shielding, and to maximize the volume available for bone graft incorporation.1 It is an exceptionally powerful tool for specific applications, such as interbody spinal fusion cages or custom cranio-maxillofacial implants, where these characteristics are the primary design drivers.
In contrast, the surface-centric paradigm, the focus of this paper, involves the strategic augmentation of a solid, high-strength core with a discrete, functionally engineered surface. The core, or substrate, is manufactured using traditional methods like forging, casting, or CNC machining from solid bar stock, which are known to produce materials with superior and more predictable bulk mechanical properties. The surface is then modified using a secondary process—such as coating or etching—to impart the desired porosity and bioactivity required for osseointegration. This methodology decouples the requirement for bulk strength from the need for surface porosity.
2.2 The Critical Engineering Trade-Off: Bulk Integrity vs. Geometric Freedom
The choice between these paradigms hinges on a critical engineering trade-off. While L-PBF provides exceptional design freedom, it comes with inherent material science consequences. The rapid heating and cooling cycles characteristic of the L-PBF process (105–107 K/s) result in a unique, non-equilibrium microstructure, typically an acicular α′ (martensite) phase in Ti-6Al-4V alloys.12 This fine-grained structure yields high ultimate tensile and yield strengths, often exceeding ASTM minimums for wrought materials.3 However, this strength comes at a significant cost: markedly reduced ductility and anisotropic mechanical properties.3 As-built L-PBF Ti-6Al-4V components frequently exhibit elongation values well below the 10% minimum required by standards like ASTM F136, necessitating post-processing heat treatments to restore some measure of ductility.13 Furthermore, the process can introduce defects such as lack-of-fusion porosity or partially melted powder particles, which can act as stress concentrators and negatively impact fatigue life.1
For highly loaded, high-cycle applications, these trade-offs are often unacceptable. A femoral hip stem, for example, must withstand millions of load cycles over its lifetime. For such an implant, fatigue strength is the paramount design consideration. The gold standard material for this application is often a forged Co-Cr-Mo alloy (e.g., ASTM F1537), which undergoes hot working to align its grain structure, resulting in exceptional fatigue resistance that is markedly superior to cast or as-built AM alternatives.4 Heavy laser etching on such stems has been implicated in early fatigue failures, highlighting the sensitivity of high-stress regions to surface modifications that create stress risers.15 In this context, a surface-only treatment that imparts porosity for fixation without compromising the integrity of the high-strength forged core is not just an alternative—it is the superior engineering choice. The same logic applies to complex anatomical trauma plates, which must be precisely contoured and possess sufficient strength and ductility to maintain fracture reduction under load.9
2.3 Croom Medical: The Technology-Agnostic Partner
Navigating these complex trade-offs requires a manufacturing partner with deep expertise across the full spectrum of production technologies. Croom Medical is uniquely positioned to provide unbiased, application-driven guidance. Our vertical integration encompasses L-PBF additive manufacturing, forging, high-precision CNC machining, and a comprehensive suite of advanced surface engineering technologies.16 Because we are not limited to a single manufacturing method, our recommendations are driven solely by the clinical and mechanical requirements of the specific implant application. This technology-agnostic approach ensures that our OEM partners are guided to the most effective and efficient manufacturing pathway for their product, all managed under a single, rigorous ISO 13485 quality management system.
2.4 A Framework for Technology Selection
To provide a clear, actionable heuristic for engineers and product managers, the following decision matrix maps common implant types to their primary requirements and the recommended manufacturing strategy. This framework illustrates the core logic of the surface-centric paradigm and serves as a guide for the technical discussions that follow.
Table 1: Framework for Selecting Porous Surface Technology
| Implant Type | Primary Mechanical Requirement | Key Biological Requirement | Dominant Geometric Feature | Recommended Primary Technology | Rationale |
| Spinal Interbody Cage | Low Modulus (to reduce stress shielding) | High Porosity for Fusion | Complex Internal Lattice | L-PBF | L-PBF excels at creating integrated, open-cell lattices that mimic bone modulus and maximize volume for bone graft.1 |
| Femoral Hip Stem | High Fatigue Strength & Wear Resistance | Proximal Osseointegration | Solid, Tapered Geometry | Forged Substrate + TPS Coating | Forged CoCr or Ti-6Al-4V provides non-negotiable fatigue life.4 Targeted TPS provides a proven ingrowth surface without compromising bulk strength.8 |
| Acetabular Cup | High Strength Shell | Porous Backing for Ingrowth | Hemispherical Shell, Polished Articulating Surface | Hybrid: L-PBF + Machining (+/- HA Coating) | L-PBF creates the porous backing efficiently.2 Precision machining creates the critical articulating surface. HA coating can accelerate early fixation.7 |
| Anatomical Trauma Plate | High Strength & Ductility | Uniform Biocompatibility | Complex, Contoured Shape | Machined Substrate + Acid Etching | CNC machining from a solid block ensures precise anatomical fit and strength.17 Acid etching provides a uniform, clean, osteoconductive surface without altering dimensions.9 |
This framework demonstrates that the optimal manufacturing strategy is not universal but is dictated by a nuanced understanding of the application’s specific bio-mechanical demands. For Tier 1 OEMs, this approach enables portfolio-wide optimization. For Tier 2 and 3 OEMs, it provides a capital-efficient pathway to developing differentiated, high-performance products by leveraging proven, robust substrates.
3. The Surface Engineering Toolbox: A Technical Deep-Dive
Mastery of implant surface engineering requires a deep, quantitative understanding of the available manufacturing technologies. Each process operates on a different physical principle and produces a surface with distinct topographical and chemical characteristics. The selection of the appropriate technology is an exercise in multi-variable optimization, balancing biological efficacy, mechanical integrity, and manufacturing feasibility. This section provides a technical overview of the primary tools in the Croom Medical surface engineering toolbox.
3.1 Additive Manufacturing (L-PBF) as the Baseline
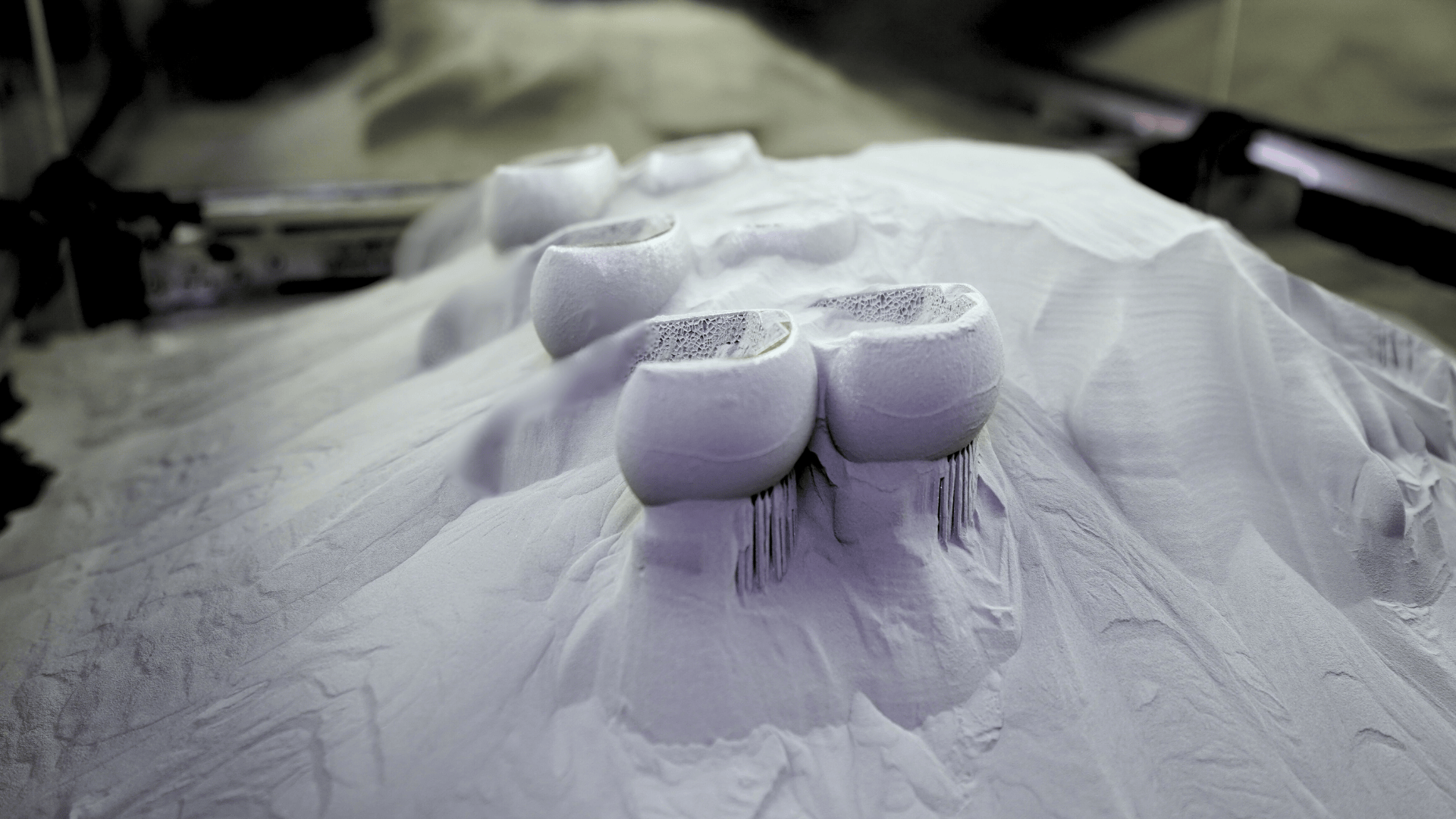
Laser Powder Bed Fusion (L-PBF) is an additive manufacturing process where a high-energy laser selectively melts and fuses thin layers of metallic powder, such as Ti-6Al-4V or commercially pure (CP) titanium, to build a three-dimensional part layer by layer.1
- Strengths: The primary advantage of L-PBF is its ability to produce highly complex geometries and integral, three-dimensional porous lattices that are impossible to create with traditional subtractive methods.2 This makes it the technology of choice for implants like interbody fusion devices, where the goal is to create a fully porous structure with a low modulus of elasticity to match that of bone and reduce stress shielding.1 The design freedom also enables the rapid production of patient-specific implants tailored to unique anatomical defects.
- Limitations and Process Control: The performance of L-PBF parts is critically dependent on the precise control of process parameters, including laser power, scanning speed, hatch spacing, and layer thickness. Unsuitable parameters can lead to defects such as incomplete fusion between powder particles or melt tracks, resulting in unwanted porosity that compromises mechanical properties.1 Achieving high densification (typically >98.5%) is essential for structural integrity.21 The as-built microstructure, characterized by fine, needle-like α′ martensite, contributes to high strength but also to lower ductility and anisotropic behavior, where mechanical properties differ based on the build direction.3 Consequently, post-processing steps are often required. These can include heat treatments (e.g., stress relief, annealing) to modify the microstructure and improve ductility, as well as surface treatments like shot blasting to remove loosely adhered, partially melted powder particles from the porous structure.2
3.2 Additive Surface Coatings: Titanium Plasma Spray (TPS) & Hydroxyapatite (HA)
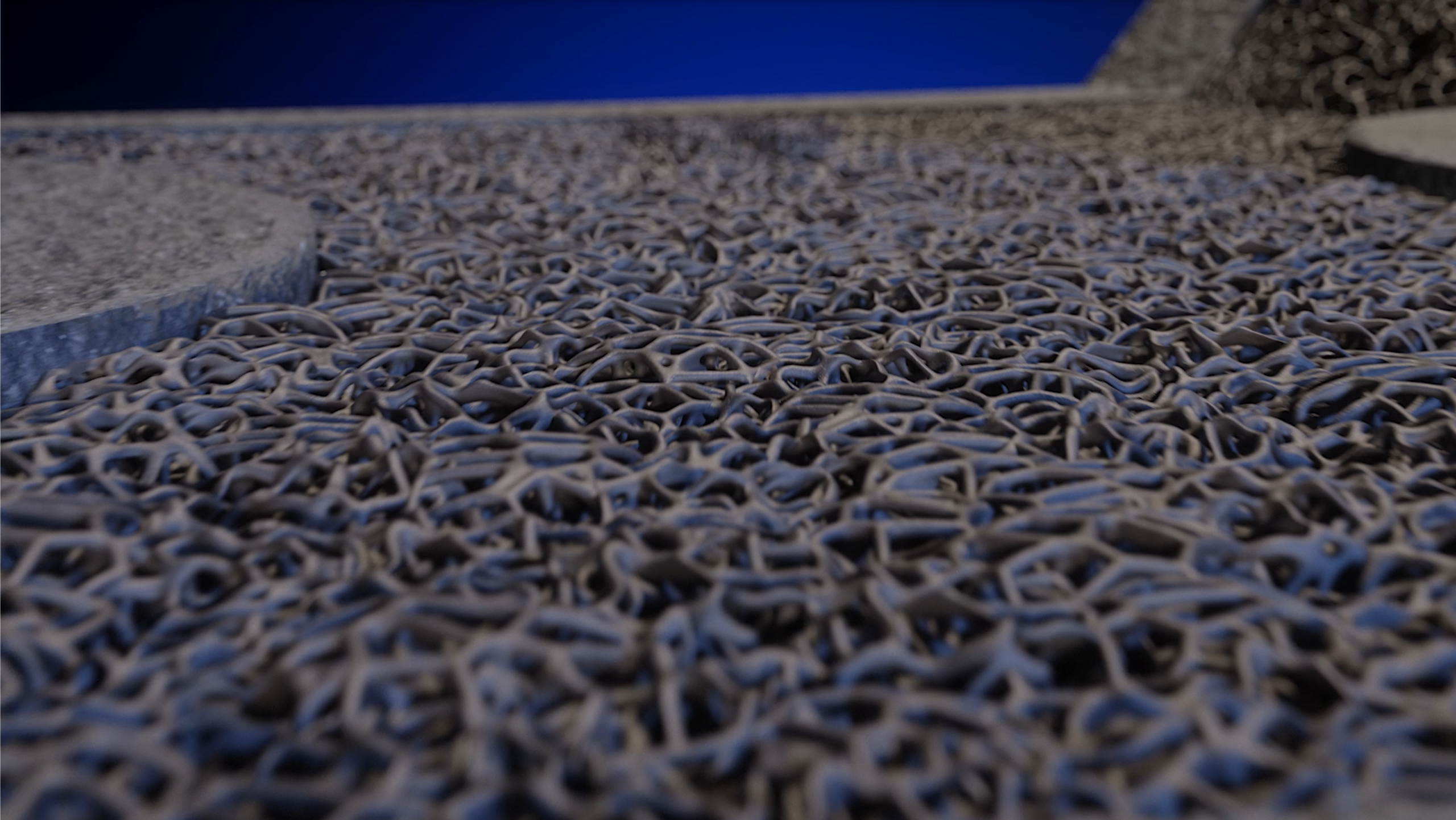
Plasma spray is an additive surface coating technology where a functional porous layer is deposited onto a solid metallic substrate. The process typically occurs in a vacuum or controlled atmosphere chamber. An inert gas, such as argon, is passed through an electric arc, ionizing it into a high-temperature, high-velocity plasma jet.8 Powdered coating material—either titanium for a porous scaffold or hydroxyapatite for bioactivity—is injected into this plasma stream. The particles are melted and propelled onto the implant substrate, where they flatten, cool rapidly, and form a strongly adhered coating.10 Prior to coating, the substrate is typically prepared by grit blasting to clean the surface and create a rough texture that enhances mechanical adhesion.2
3.2.1 Titanium Plasma Spray (TPS)
TPS coatings are designed to create a rough, porous, and biocompatible surface that promotes long-term, stable biological fixation through osseointegration.5 The primary mechanism is mechanical interlocking, where new bone grows into the interconnected pores of the coating, anchoring the implant securely.8
- Key Parameters and Outputs:
- Coating Material: The powders used are typically unalloyed titanium or Ti-6Al-4V alloy, which must meet the chemical and physical requirements of standards such as ASTM F1580, “Standard Specification for Titanium and Titanium-6 Aluminum-4 Vanadium Alloy Powders for Coatings of Surgical Implants”.23
- Applicable Substrates: TPS is a versatile process that can be applied to a variety of medical-grade substrates, most commonly Ti-6Al-4V but also high-strength Cobalt-Chrome (CoCr) alloys, enabling porous surfaces on implants where L-PBF is not a viable option.11
- Coating Thickness: Typical coating thicknesses range from 250 µm to 750 µm (0.010–0.030 inches).11 Some specifications allow for thicknesses up to 800 µm, though it is noted that thicknesses beyond 500 µm may not significantly improve adhesion strength.8 FDA guidance for porous coatings suggests a range of 500 to 1,500 µm.26
- Porosity and Pore Size: The interconnected porosity is a critical functional attribute. Typical porosity levels are in the range of 20% to 50%.8 A porosity of approximately 30-35% is common and has demonstrated excellent clinical results.27 The pore size is engineered to be optimal for bone ingrowth, with typical ranges cited as 100–250 µm or 75–300 µm.8 This size is sufficient for the formation of mineralized bone and vascularization within the coating structure.
- Surface Roughness (Ra): TPS coatings are inherently rough, a key factor for achieving initial press-fit stability. Average surface roughness (Ra) values typically range from 3.5 µm to as high as 80 µm.8
- Coating Bond Strength: The adhesion of the coating to the substrate is a critical performance metric. Bond strength is quantified using standardized mechanical tests. Per FDA guidance, the static tensile strength should exceed 22 MPa, and the static shear strength should exceed 20 MPa.28 Industry-standard TPS coatings routinely demonstrate tensile bond strengths greater than 34.5 MPa (5000 psi), with values reaching up to 100 MPa.8 These properties are validated according to ASTM F1147, “Standard Test Method for Tension Testing of Calcium Phosphate and Metallic Coatings,” and ASTM F1044, “Standard Test Method for Shear Testing of Calcium Phosphate Coatings and Metallic Coatings”.29
3.2.2 Hydroxyapatite (HA) Coating
Hydroxyapatite (Ca10(PO4)6(OH)2) is a calcium phosphate ceramic that is the primary inorganic mineral component of natural bone.31 When applied as a coating, it provides an osteoconductive surface, meaning it actively supports the migration, attachment, proliferation, and differentiation of bone-forming cells (osteoblasts), thereby accelerating the process of bone apposition and bonding at the implant-tissue interface.19
- Key Parameters and Outputs:
- Coating Material: The quality of the HA coating is highly dependent on the purity of the starting powder. High-purity HA powder conforming to ASTM F1185, “Standard Specification for Composition of Hydroxyapatite for Surgical Implants,” is required.33
- Coating Thickness: HA coatings are typically thinner than TPS coatings. Customizable thickness ranges include thin (5–15 µm), nominal (20–40 µm), and thick (35–70 µm).33 The thickness is carefully controlled, as thicker coatings can have higher residual stress, potentially impacting bond strength.33
- Phase Purity and Crystallinity: These are perhaps the most critical attributes for HA coating performance. The plasma spray process can cause thermal decomposition of HA into other, more soluble calcium phosphate phases. High phase purity, with a minimum of 90% HA, is desirable.33 Crystallinity is also crucial; highly crystalline HA is more stable and resorbs more slowly and predictably in the body. Amorphous or low-crystallinity phases can dissolve too quickly, compromising the long-term stability of the interface.19 FDA guidance specifies a minimum crystallinity of 62%, which is validated using X-ray diffraction (XRD) per ASTM F2024.33
- Coating Bond Strength: The bond strength of HA coatings is a subject of considerable research. While HA promotes excellent bioactivity, its bond to the metallic substrate can be a point of weakness. Long-term immersion in simulated body fluids (SBF) has been shown to decrease the bond strength of some HA coatings due to cohesive degradation.22 Per ISO 13779-4, the mean tensile adhesion strength should be no less than 15 MPa, with no individual result below 10 MPa.26 Testing is conducted according to ASTM F1147.33
3.3 Subtractive Surface Modification: Validated Acid Etching
Unlike additive coatings, acid etching is a subtractive surface modification process. It involves the controlled immersion of a titanium or titanium alloy implant in a heated, aggressive acid solution (such as a mixture of hydrochloric and sulfuric acids) for a specified time and temperature.35 This process chemically removes a thin layer of the native oxide and underlying metal, creating a complex, uniform micro- and nano-scale topography directly on the substrate material.
Resulting Topography: The etching process transforms a relatively smooth machined surface into one characterized by a network of irregular, sub-micron to micron-sized pits (typically 0.5–3 µm) and other complex features.9 This creates a high-surface-area, nanostructured topography without adding a distinct material layer.36
- Biological Advantage: This precisely controlled micro- and nano-roughness has been proven to be highly effective at modulating cellular response. The topography increases surface energy and wettability, which are critical for the initial adsorption of proteins (like fibronectin and vitronectin) from the blood. This protein layer, in turn, mediates the attachment, spreading, and proliferation of osteoblasts.9 Studies have shown that osteoblast differentiation and the expression of bone-specific genes are significantly enhanced on acid-etched surfaces compared to smooth, machined surfaces.39
- Engineering Advantage: A critical advantage of acid etching is that it preserves the precise macroscopic dimensions and tolerances of the underlying component. Because it is a non-contact, uniform chemical process, it can be applied to highly complex, finished parts without altering their critical anatomical fit. This makes it the ideal surface treatment for devices like anatomically contoured trauma plates, bone screws, and dental implants, where dimensional accuracy is paramount.16 It also produces an exceptionally clean surface, free from the potential contaminants of abrasive blasting media.20
3.4 Hybrid & Machined Surfaces: Engineering Hierarchical Topographies
The frontier of surface engineering lies in the creation of “hierarchical” topographies—surfaces that are deliberately structured at multiple length scales to mimic the complex architecture of natural bone.41 This advanced approach moves beyond simply creating random roughness and instead involves the intelligent design of surface features to guide tissue organization and cellular function at different levels.
Concept and Process: A hierarchical surface is typically created by combining two or more manufacturing processes. For instance, high-precision CNC machining or laser surface texturing can be used to create well-defined macro-scale features on the implant surface, such as parallel grooves, channels, or dimples with dimensions greater than 10 µm.17 These larger features can provide contact guidance for tissue organization and improve initial mechanical stability. Subsequently, a secondary process like acid etching or anodization is applied to the entire surface. This superimposes a
micro- and nano-scale roughness onto the larger, machined features.42
- Functional Benefit: This multi-scale topography is hypothesized to provide synergistic biological benefits. The macro-features guide the overall organization of the healing tissue, while the micro- and nano-textures provide the optimal environment for protein adsorption and individual cell attachment and differentiation.42 This combination can lead to faster and more robust osseointegration than a surface with a single-scale topography. This represents a paradigm shift from surface modification to true surface engineering, offering a powerful tool for developing next-generation implants with tailored, performance-enhancing interfaces.
3.5 Comparative Analysis
The selection of the most appropriate surface engineering technology is a critical design decision. The following table provides a comparative analysis of the key technical and functional attributes of the technologies discussed.
Table 2: Comparative Analysis of Surface Engineering Technologies
| Feature | L-PBF (Integral Porosity) | Titanium Plasma Spray (TPS) | Hydroxyapatite (HA) Coating | Acid Etching | Hybrid (Machined + Etched) |
| Process Type | Additive (Monolithic) | Additive (Coating) | Additive (Coating) | Subtractive (Modification) | Subtractive + Subtractive |
| Primary Mechanism | Bulk Porosity | Mechanical Interlock | Osteoconduction | Micro/Nano Topography | Hierarchical Topography |
| Typical Feature Size | 100-1000 µm (Lattice) | 75-300 µm (Pores) | N/A (Bioactive Layer) | 0.5-3 µm (Pits) | Macro (>10µm) + Micro/Nano |
| Effect on Bulk Properties | Defines all properties; lower ductility/fatigue vs. wrought 3 | Minimal thermal effect; less fatigue reduction than sintering 8 | Minimal thermal effect | None; preserves substrate integrity | None; preserves substrate integrity |
| Key Advantage | Unmatched geometric freedom; integrated porosity 2 | Proven, robust ingrowth surface; applicable to CoCr 11 | Accelerates early bone apposition 32 | Preserves precise dimensions; uniform, clean surface 20 | Multi-scale biological guidance; optimized design 42 |
| Key Limitation | Mechanical property trade-offs; post-processing needed 12 | Line-of-sight process; potential for particle delamination | Potential for resorption; bond strength degradation 22 | Limited to reactive metals (Ti); less macro-roughness | Increased process complexity and cost |
| Ideal Application | Spinal Cages, Custom Cranial Implants | Femoral Stems, Acetabular Shells | Spinal Implants, Dental Screws | Trauma Plates, Dental Implants | Next-gen joint replacements, spinal hardware |
This comparative framework underscores that there is no single “best” technology. The optimal choice is contingent on a detailed analysis of the implant’s specific performance requirements. An engineering team must weigh the need for geometric complexity against the demand for fatigue strength, and the desire for accelerated bioactivity against the need for long-term mechanical stability. True expertise lies not in advocating for one process, but in understanding the entire toolbox and selecting the right combination of tools for the clinical application at hand.

4. The Croom Medical Difference: An Integrated Validation Framework
Providing a comprehensive toolbox of surface engineering technologies is only one part of the equation. Delivering safe, effective, and reliable orthopaedic implants requires a robust, integrated framework for process control, validation, and quality assurance. Croom Medical’s key differentiator lies in our ability to seamlessly combine these advanced manufacturing processes with rigorous in-house characterization and a comprehensive quality management system, offering our OEM partners a de-risked, streamlined path from concept to market.
4.1 Application-Driven Technology Selection
Our engagement with an OEM partner does not begin with a discussion of a specific manufacturing process. It begins with a deep, collaborative analysis of the clinical application and its associated bio-mechanical demands. We work with our partners’ R&D and product development teams to define the critical performance attributes of the implant: What are the primary and secondary load cases? What is the required fatigue life? Is rapid initial fixation or long-term mechanical stability the priority? What is the target patient population and bone quality?
Only after a thorough understanding of these requirements do we co-engineer the optimal manufacturing pathway. This application-driven approach ensures that technology selection is a conclusion based on evidence, not a predetermined starting point. This consultative process is particularly valuable for our diverse OEM partners. For Tier 1 OEMs, it facilitates the optimization of large product portfolios, ensuring the right technology is used for the right product line to balance performance and cost. For Tier 2 OEMs, it enables the development of highly differentiated products that can compete on performance without massive capital investment in a single technology. For Tier 3 and start-up companies, it provides a clear, efficient, and scientifically sound manufacturing and regulatory strategy, accelerating time-to-market.44
4.2 In-House Surface Characterization & Validation
Trust in a manufacturing process is built on data. Croom Medical maintains a state-of-the-art, in-house materials science laboratory dedicated to the characterization and validation of our implant surfaces. This capability is not merely for final inspection; it is an integral part of our process development and control loop, ensuring that every surface we produce meets stringent quantitative specifications. Our key validation techniques include:
Morphological and Topographical Analysis: We utilize Scanning Electron Microscopy (SEM) to provide high-resolution imaging of surface morphology. SEM allows for detailed visualization of the interconnected porosity of a TPS coating, the uniformity of an acid-etched surface, or the integrity of an HA layer.47 For precise, three-dimensional quantitative analysis of surface roughness, we employ non-contact methods like White Light Interferometry or Laser Confocal Microscopy. These techniques provide critical parameters such as average roughness (Ra) and peak-to-valley height (Rz), allowing us to ensure that surface topography meets design specifications.49
- Interface and Microstructure Analysis: The integrity of the interface between a coating and its substrate is critical to its performance. We use metallographic techniques to analyze this interface in cross-section. Specimens are sectioned, mounted in resin, and meticulously polished and etched. This allows for microscopic examination of the coating-substrate bond, confirming, for example, the presence of a true metallurgical bond in a TPS coating or the absence of cracks and delamination at the base of an HA coating.27
- Mechanical Testing: To quantify the mechanical performance of our coatings, we conduct standardized adhesion and cohesion tests. The tensile strength of coatings is measured using a pull-off test according to ASTM F1147, where a fixture is bonded to the coated surface and pulled in tension until failure.29 This test determines whether failure occurs within the coating (cohesive failure) or at the coating-substrate interface (adhesive failure) and quantifies the bond strength in megapascals (MPa). Similarly, the shear strength is measured according to ASTM F1044, providing critical data on the coating’s resistance to parallel forces.30 These tests provide the empirical data needed to validate that our coatings exceed FDA and industry requirements.28
4.3 Integrated Manufacturing & Quality Workflow
The true power of Croom Medical’s approach lies in the seamless integration of these advanced surface processes into a single, validated manufacturing chain, all governed by one comprehensive Quality Management System (QMS) certified to ISO 13485:2016.53 This international standard for medical device manufacturing mandates rigorous controls over the entire product lifecycle, from design and development to production, distribution, and post-market surveillance.55
For an OEM partner, this integrated model offers a profound strategic advantage over managing a fragmented supply chain of disparate vendors. Consider the typical workflow for a coated, forged implant:
Workflow: Forged & Coated Femoral Stem
- 1. Material Sourcing: Procure certified CoCrMo billet (e.g., ASTM F1537).
- 2. Forging: Hot forge billet to near-net shape.
- 3. CNC Machining: Machine the forged blank to final dimensions, including the critical polished neck and trunnion.
- 4. Surface Preparation: Mask critical surfaces to protect them from subsequent steps.
- 5. Grit Blasting: Prepare the proximal body for coating.
- 6. Coating: Apply TPS coating via vacuum plasma spray in a validated process.
- 7. Post-Coating: Unmask the component.
- 8. Final Inspection: Conduct 100% dimensional and visual inspection.
- 9. Cleaning & Packaging: Perform validated cleaning, passivation, and sterile packaging.
In a traditional, outsourced model, each of these steps could represent a different vendor, a different quality system, and a different point of potential failure, delay, or miscommunication. At Croom Medical, this entire sequence is managed as a single, continuous process within one facility and under one QMS. This provides end-to-end traceability, with every process parameter and inspection result documented in the device history record. It drastically reduces logistical complexity, shortens lead times, and simplifies supply chain management for the OEM. Most importantly, it consolidates accountability. There is a single point of responsibility for the quality and performance of the final device, eliminating the risk and ambiguity inherent in a multi-vendor supply chain.56 This integrated framework is our commitment to providing not just advanced manufacturing, but also certainty, reliability, and a strategic partnership that de-risks the path to market.
5. Case Studies: The Right Surface for the Right Application
The theoretical advantages of a multi-technology, surface-centric approach are best illustrated through its application to real-world engineering challenges. The following case studies demonstrate how Croom Medical’s integrated platform is used to develop optimized implants that would be impossible to achieve with a single manufacturing methodology.
5.1 High-Strength Application: The Coated Forged Hip Stem
The Challenge: To engineer a femoral hip stem for cementless fixation intended for a long, active clinical life. The primary engineering requirement is maximum fatigue resistance to prevent implant fracture, which is a catastrophic failure mode. A secondary requirement is a durable, porous surface on the proximal aspect of the stem to ensure stable and permanent biological fixation.
The Substrate Solution: The substrate material and manufacturing method are chosen to maximize fatigue life. A Cobalt-Chrome-Molybdenum (CoCrMo) alloy conforming to ASTM F1537 is selected. The implant blank is created via hot forging, a process that works the metal to create a refined and aligned grain structure. This process results in significantly enhanced fatigue strength and ductility compared to as-cast or as-built AM materials, making it the ideal choice for this high-cycle, high-load application.4 The fatigue strength of hot-forged Co-Cr-Mo alloy can reach approximately 1000 MPa at 107 cycles, providing a robust foundation for the implant.4
- The Surface Solution: After the forged blank is CNC machined to its final, precise geometry, a targeted surface modification is applied. The highly polished neck and trunnion, critical for minimizing wear against the femoral head, are masked. The proximal body of the stem is then coated with Titanium Plasma Spray (TPS). This process deposits a porous layer of commercially pure titanium, typically 300-500 µm thick with 30-40% interconnected porosity, creating a proven scaffold for bone ingrowth.8 The TPS process has a minimal thermal effect on the underlying forged substrate, preserving its superior mechanical properties.8
- The Result: An optimized, bio-mechanically superior implant that leverages the best of both worlds. It combines the non-negotiable fatigue strength of a forged CoCr substrate with the proven, durable osseointegration capabilities of a TPS coating. This “no-compromise” design is a direct result of the surface-centric paradigm, achieving a level of performance and safety that a monolithic AM approach cannot match for this specific application.
5.2 Biocompatibility & Precision Application: The Etched Titanium Trauma Plate
The Challenge: To manufacture a complex, low-profile anatomical plate for the fixation of a distal radius fracture. The implant must feature multiple, precisely located screw holes and a contoured shape that perfectly matches the complex anatomy of the bone to avoid soft tissue irritation. Furthermore, the entire bone-contacting surface must be optimized to promote rapid and reliable healing.
The Substrate Solution: The only manufacturing method capable of achieving the required dimensional precision and complex geometry is high-precision CNC machining. The plate is milled from a solid block of medical-grade Ti-6Al-4V ELI (Extra Low Interstitial) alloy. This ensures absolute control over every contour, hole diameter, and edge profile, resulting in an implant that fits the anatomy perfectly and minimizes stress concentrations.17
- The Surface Solution: After machining and a thorough cleaning process, the entire trauma plate is subjected to a validated acid etching process. Immersion in a heated acid solution uniformly removes a microscopic layer of material from all surfaces, creating a clean, consistent micro- and nano-scale topography.20 This process increases surface energy and creates features that are highly conducive to osteoblast adhesion and proliferation, effectively transforming the entire surface from bio-inert to bioactive.9
- The Result: An implant that excels in both mechanical function and biological response. The CNC-machined core guarantees the anatomical fit and strength required for fracture stability. The acid-etched surface enhances the biological performance across the entire implant without altering any of its critical dimensions. This case study highlights how a relatively simple, cost-effective subtractive surface modification can add significant clinical value to a high-precision component, representing an ideal manufacturing pathway for many trauma and extremity devices.
5.3 Hybrid Innovation: The AM-Machined-Coated Acetabular Cup
The Challenge: To create a cutting-edge acetabular cup for total hip arthroplasty that addresses three distinct design goals simultaneously: a highly porous, bone-like backing for robust cementless fixation; a perfectly smooth, low-friction inner articulating surface to minimize polyethylene wear and osteolysis; and enhanced bioactivity to accelerate early bone apposition.
- The Multi-Technology Solution: This complex challenge requires a hybrid manufacturing approach that combines the strengths of multiple advanced technologies in a single, integrated workflow.
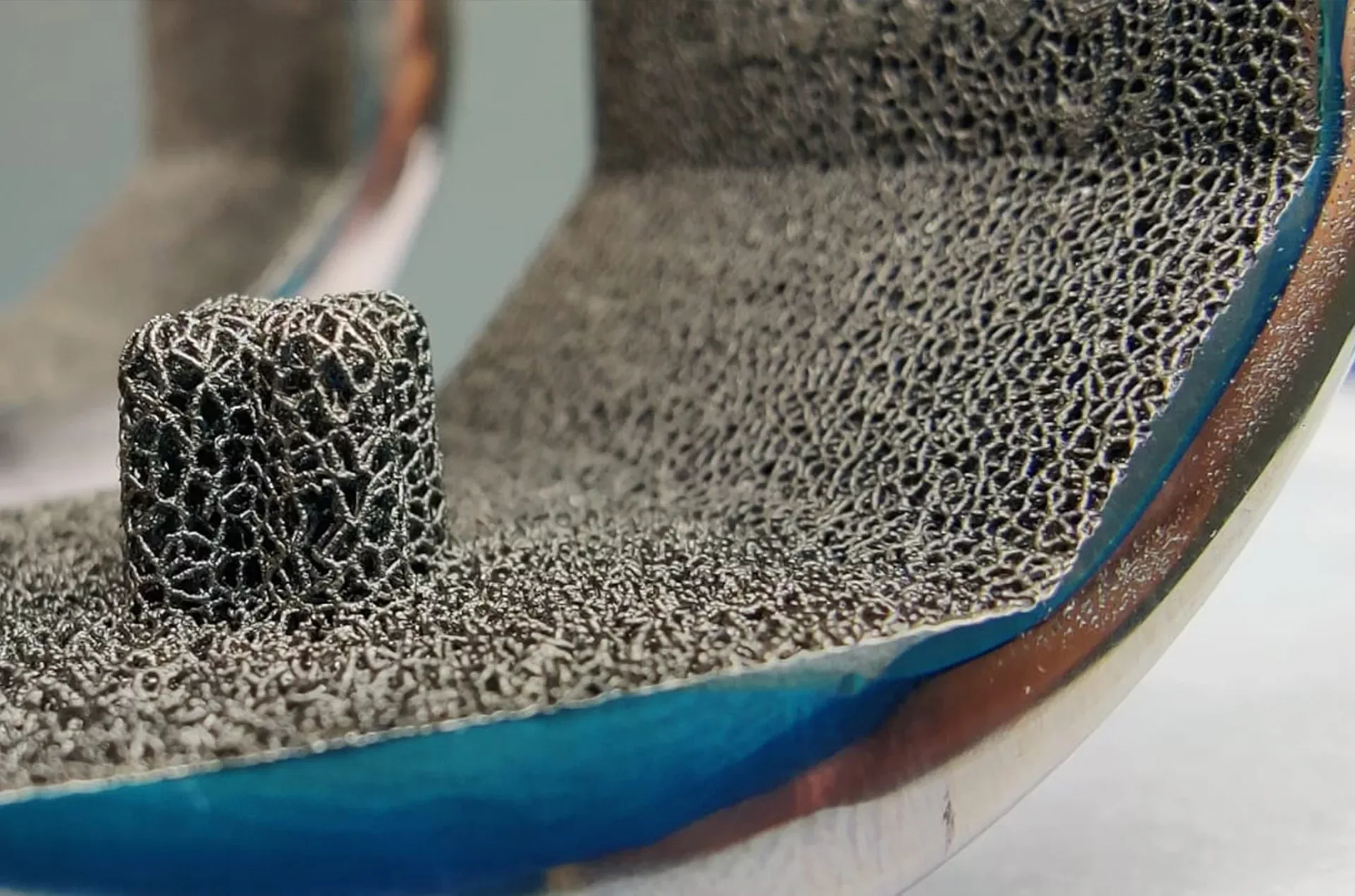
- Additive Manufacturing (L-PBF): The process begins with L-PBF to create the basic shell of the cup from Ti-6Al-4V powder. The key advantage here is the ability to print an integral, three-dimensional trabecular lattice structure on the back side of the cup, mimicking the structure of cancellous bone. This is the most efficient method for creating such a complex porous feature.2
- Precision Machining: The as-printed cup is then transferred to a high-precision CNC lathe. The inner, articulating surface is diamond-turned to an exceptionally smooth, mirror-like finish (with a surface roughness, Ra, in the sub-micron range). This step is critical for ensuring low-wear performance against the polyethylene liner, a key factor in the long-term survival of the joint replacement.58
- Additive Coating: As a final step, the cup is selectively coated. The highly polished inner surface is masked, and a thin (e.g., 20-40 µm) layer of crystalline Hydroxyapatite (HA) is applied to the porous lattice structure on the back side using plasma spray.33
- The Result: A truly hybrid, “best-of-all-worlds” implant that achieves performance levels unattainable by any single process. L-PBF provides the ideal macro-porous scaffold for bone ingrowth. Precision machining creates the optimal tribological surface for low wear. And the HA coating provides an osteoconductive stimulus to accelerate early biological fixation and enhance initial stability.19 This case study serves as a powerful demonstration of Croom Medical’s capability to integrate the most advanced manufacturing technologies to solve complex, multi-faceted design challenges.

6. Conclusion: Engineering the Bio-Mechanical Interface
The paradigm of orthopaedic implant design is undergoing a fundamental shift. For decades, the focus was primarily on bulk material properties and macroscopic shape. Today, it is clear that long-term clinical success is determined at the interface—the microscopic and nanoscopic landscape where the implant meets the living biological system.5 Advanced implant design is no longer just about the part’s geometry; it is about the deliberate, multi-scale engineering of this critical bio-mechanical interface. Croom Medical offers the complete, validated, and vertically integrated toolbox to achieve this.
By moving beyond a “one-size-fits-all” approach and embracing a surface-centric philosophy, we provide R&D engineers, materials scientists, and product development managers with a powerful set of strategic advantages:
Uncompromised Mechanical Integrity: The ability to select the optimal substrate—whether it be forged CoCr for maximum fatigue life or machined titanium for precision—ensures that the implant’s bulk properties are never sacrificed. The core of the implant can be engineered to handle its specific mechanical loads without compromise.
- Tailored Biological Responses: With a comprehensive suite of surface technologies, from additive coatings like TPS and HA to subtractive modifications like acid etching, the implant surface can be precisely tailored to elicit the desired biological response—be it rapid osteoconduction, durable mechanical ingrowth, or uniform biocompatibility.
- Expanded Design Freedom: By decoupling bulk material properties from surface characteristics, engineers are freed from the limitations of a single manufacturing process. This opens the door to creating novel, hybrid implants that leverage the best attributes of multiple materials and processes, pushing the boundaries of performance and innovation.
- De-risked and Streamlined Path to Market: Our integrated, ISO 13485-certified workflow provides a single point of accountability, simplifying the supply chain, reducing risk, and accelerating development timelines for our OEM partners.
The era of choosing a single manufacturing process is over. The future belongs to those who can masterfully combine them. Croom Medical possesses the technology, the expertise, and the integrated framework to partner with you in engineering the next generation of orthopaedic implants.
Challenge our engineers. Bring us your most demanding implant application and let’s co-engineer the optimal surface solution together.
References:
1. 1 Haase, C., et al. (2023). Additive manufacturing of titanium-based alloys for medical applications: Process optimization for minimizing porosity and development of a new biocompatible alloy.
Frontiers in Bioengineering and Biotechnology, 11, 1260925.
2. 2 Arjunan, A., et al. (n.d.). Analysis of the Porous Structures from Laser Powder Bed Fusion Additive Manufacturing.
ResearchGate.
3. 21 Vamsi Krishna, B., et al. (2022). Additive Manufacturing of Biocompatible Ti–35Nb–7Zr–5Ta Alloy for Patient-Specific Orthopedic Implants.
ACS Omega, 7(11), 9846-9855.
4. 22 Yusop, A. H., et al. (2015). Surface Modification of Titanium Dental Implants: A Review.
BioMed Research International, 2015, 791725.
5. 10 Jaworska, L., et al. (2018). Titanium Plasma-Sprayed Coatings on Polymers for Hard Tissue Applications.
Materials, 11(12), 2536.
6. 11 Orchid Orthopedic Solutions. (n.d.). TPS Technical Information Sheet.
7. 19 Velasquez, P., et al. (2008). Hydroxyapatite coatings.
Revista Española de Cirugía Ortopédica y Traumatología (English Edition), 52(4), 244-249.
8. 31 Farooq, U., et al. (2023). A comprehensive review on hydroxyapatite coated metallic implants for biomedical applications.
Ceramics International, 49(1), 1-17.
9. 33 Himed. (n.d.). Superior Hydroxyapatite Coatings for Medical Implants.
10. 32 Number Analytics. (n.d.). Hydroxyapatite Coating in Joint Replacement.
11. 16 ALM Ortho. (n.d.). Osseointegration.
12. 35 Al-Hity, R., et al. (2016). The influence of different acids etch on dental implants titanium surface.
IOSR Journal of Dental and Medical Sciences, 15(8), 87-91.
13. 63 Suzuki, T., et al. (2015). Effect of ultraviolet photoactivation of titanium on osseointegration in a rat model.
Biomaterials, 53, 390-401.
14. 17 Acrotec Medtech. (n.d.). The role of CNC machining, laser techniques, and surface treatments in manufacturing orthopaedic and trauma implants.
15. 7 Lin, Y.-C., et al. (2024). Discrepancies of full-arch implant-supported titanium frameworks fabricated by hybrid additive-subtractive manufacturing vs. conventional milling.
Scientific Reports, 14(1), 11468094.
16. 58 Croom Medical. (n.d.). Advanced Polishing Techniques in Joint Replacement Manufacturing.
17. 13 S-L., M., et al. (2022). A Review of Ti6Al4V Additive Manufacturing by Laser Powder Bed Fusion: The Interplay between Process, Microstructure, and Mechanical Properties.
Materials, 15(12), 4249.
18. 12 Liu, C., et al. (2024). Microstructure, mechanical properties and post-machining performance of LPBF Ti–6Al–4V alloys: a review.
Computer-Aided Design and Applications, 21(3), 441-467.
19. 3 Murr, L. E., et al. (2015). Microstructure and Mechanical Properties of Wrought and Additive Manufactured Ti-6Al-4V Cylindrical Bars.
Journal of Materials Science & Technology, 31(7), 681-688.
20. 64 Advanced Refractory Metals. (n.d.). An Introduction to Porous Tantalum Implants.
21. 65 Li, Y., et al. (2007). Mechanical properties of titanium–tantalum alloys for biomedical application.
Materials Transactions, 48(3), 261-265.
22. 66 Various Authors. (n.d.). Titanium or Tantalum?
ResearchGate.
23. 5 Wikipedia. (n.d.). Osseointegration.
24. 67 Wu, W., et al. (2024). Porous PEEK for Orthopedic Applications: A Review.
Polymers, 17(14), 1968.
25. 68 Sacks, J. M., et al. (2012). Osseointegration.
Techniques in Orthopaedics, 27(4), 349-352.
26. 29 ASTM International. (1999). ASTM F1147-99: Standard Test Method for Tension Testing of Calcium Phosphate and Metallic Coatings.
27. 34 Endolab. (n.d.). Tensile strength of coatings.
28. 51 ANSI Webstore. (2017). ASTM F1147-05(2017)e1: Standard Test Method for Tension Testing of Calcium Phosphate and Metallic Coatings.
29. 69 Various Authors. (n.d.). Adhesion test results according to ASTM F1147-99.
ResearchGate.
30. 23 ANSI Webstore. (2018). ASTM F1580-18: Standard Specification for Titanium and Titanium-6 Aluminum-4 Vanadium Alloy Powders for Coatings of Surgical Implants.
31. 30 TestResources. (n.d.). ASTM F1044 Shear Testing for Calcium Phosphate and Metallic Coatings.
32. 24 Laboratuar.com. (n.d.). ASTM F1580-12 Standard Specification for Titanium and Titanium-6 Aluminum-4 Vanadium Alloy Powders for Coatings of Surgical Implants.
33. 52 DIN Media. (n.d.). ASTM F 1044:2018.
34. 47 Number Analytics. (n.d.). The Ultimate Guide to Surface Analysis of Biomaterials for Orthopedic Implants.
35. 48 Knez, K., et al. (2021). Advanced Analytical Techniques for the Characterization of Bioactive Coatings on Medical Implants.
Molecules, 26(24), 7594.
36. 70 Various Authors. (n.d.). Surface characterization.
ResearchGate.
37. 18 Acrotec Medtech. (n.d.). Orthopedic Implant Contract Manufacturing.
38. 25 Orchid Orthopedic Solutions. (n.d.). TPS (Titanium Plasma Spray) Coating Technical Information Sheet.
39. 28 U.S. Food and Drug Administration. (n.d.). Guidance for Industry on Testing of Metallic Plasma Sprayed Coatings on Orthopedic Implants to Support Reconsideration of Postmarket Surveillance.
40. 27 Exactech. (2006). Titanium Plasma Spray: A Proven Technology for Cementless Fixation.
41. 8 DOT America. (n.d.). Titanium Plasma Spray (TPS) Implant Surfaces For Cementless Anchoring.
42. 34 Endolab. (n.d.). Tensile strength of coatings.
43. 33 Himed. (n.d.). Superior Hydroxyapatite Coatings for Medical Implants.
44. 26 U.S. Food and Drug Administration. (2024). Content of Premarket Submissions for Metallic and Calcium Phosphate Coated Orthopedic Implants – Draft Guidance.
45. 71 O’Neill, L. (2012). Development of a Novel Biocompatible Abrasive and Coating for Medical Implant Applications.
UCD Research Repository.
46. 37 Olivares-Navarrete, R., et al. (2016). Regulation of Osteoblast Differentiation by Acid-Etched and/or Grit-Blasted Titanium Substrate Topography Is Enhanced by 1,25(OH)2D3 in a Sex-Dependent Manner.
PLoS ONE, 11(10), e0165296.
47. 38 Lukaszewska-Kuska, M., et al. (2021). The Effects of Titanium Topography and Chemical Composition on Human Osteoblast Cell.
Materials, 14(10), 2589.
48. 39 Lukaszewska-Kuska, M., et al. (2022). The Effects of Titanium Topography and Chemical Composition on Human Osteoblast Cell.
International Journal of Molecular Sciences, 23(3), 1695.
49. 72 Various Authors. (n.d.). The hierarchical structure of a typical implant surface.
ResearchGate.
50. 43 Li, J., et al. (2023). Polyetheretherketone implants with hierarchical porous structure for boosted osseointegration.
Journal of Nanobiotechnology, 21(1), 229.
51. 41 Gittens, R. A., et al. (2018). The role of surface topography on the behaviour of cells on titanium-based biomaterials.
Journal of Materials Chemistry B, 6(25), 4167-4182.
52. 73 Number Analytics. (n.d.). The Ultimate Guide to Orthopedic Implants: Surface Modification.
53. 42 Han, C.-M., et al. (2020). Multi-Scale Surface Treatments of Titanium Implants for Rapid Osseointegration: A Review.
Journal of Clinical Medicine, 9(7), 2115.
54. 74 Zhang, L., et al. (2019). Additive Manufacturing of Customized Metallic Orthopedic Implants: Materials, Structures, and Surface Modifications.
Metals, 9(9), 986.
55. 75 Vincent Metals. (n.d.). ASTM F1537 Cobalt Chrome.
56. 14 Lork Group. (n.d.). Cobalt-Chrome Alloys: Properties, Applications, and Common Variants.
57. 4 Niinomi, M., et al. (2012). Comparison of Fatigue Properties and Fatigue Crack Growth Rates of Various Implantable Metals.
Materials, 5(12), 2985-3004.
58. 15 Gilbert, J. L., et al. (2001). Early fatigue failures of cemented, forged, cobalt-chromium femoral stems at the neck-shoulder junction.
The Journal of Arthroplasty, 16(2), 234-239.
59. 9 Velasco-Ortega, E., et al. (2016). Effect of Hydrofluoric Acid Etching Time on Titanium Topography, Chemistry, Wettability, and Cell Adhesion.
PLoS ONE, 11(10), e0165296.
60. 40 Doe, Y., et al. (2018). Titanium surface treatment by calcium modification with acid-etching promotes osteogenic activity and stability of dental implants.
Journal of the Mechanical Behavior of Biomedical Materials, 88, 289-297.
61. 36 Hsu, H.-C., et al. (2017). The Effects of Acid Etching on the Nanomorphological Surface Characteristics and Activation Energy of Titanium Medical Materials.
Coatings, 7(11), 188.
62. 20 Valarezo, G. M., et al. (2025). Acid Etching as an Alternative to the SLA Method for Treating the Surface of Ti Dental Implants.
Materials, 18(7), 1632.
63. 76 Kaczmarek, M., et al. (2025). Long-Term Outcomes of Total Hip Arthroplasty with the L-Cup Acetabular Component: A Retrospective Analysis.
Journal of Clinical Medicine, 14(4), 1301.
64. 59 Kim, Y.-H., et al. (2015). Long-term Results of Total Hip Arthroplasty Using Hydroxyapatite-Coated Acetabular Cup.
Hip & Pelvis, 27(4), 209-215.
65. 77 Hailer, N. P., et al. (2010). Uncemented HA-coated cups in primary hip arthroplasty: a study of 8,043 cases from the Swedish Hip Arthroplasty Register.
Acta Orthopaedica, 81(2), 166-173.
66. 47 Number Analytics. (n.d.). The Ultimate Guide to Surface Analysis of Biomaterials for Orthopedic Implants.
67. 49 Various Authors. (n.d.). White light interferometry microscopy 3D images and surface profile characteristics.
ResearchGate.
68. 50 O’Hara, S. P., et al. (2022). Transcriptional Responses of Mesenchymal Stromal/Stem Cells to Clinically Relevant Titanium Biomaterials Reveal a Role for the Integrated Stress Response in Regulating Cell-Biomaterial Interactions.
The American Journal of Pathology, 192(1), 101-115.
69. 78 Various Authors. (2025). Enhancing Osseointegration in Dental Implants: A Review of Surface Treatment Methods for Titanium and Zirconia.
Materials, 18(3), 320.
70. 53 NQA. (2020). How to Implement ISO 13485.
71. 55 Quality Forward. (n.d.). ISO 13485 in Medical Device Manufacturing.
72. 54 Cognidox. (n.d.). ISO 13485: The Definitive Guide for Medical Device Developers.
73. 44 OrthoMaterials. (n.d.). Market Data.
74. 45 Market.us. (2025). Orthopedic Contract Manufacturing Market News.
75. 79 Data Bridge Market Research. (2024). Global Orthopedic Devices Market.
76. 80 ORTHOWORLD Inc. (n.d.). Orthopedic Market Size and Share.
77. 81 Global Market Insights. (n.d.). Orthopedic Contract Manufacturing Market.
78. 82 The OrthoForum. (n.d.). Business of Orthopaedics.
79. 83 Intrepy Healthcare Marketing. (2023). 10 Orthopedic Marketing & Advertising Ideas 2023.
80. 84 Weave. (n.d.). Orthopedic Marketing: 10 Strategies for Your Practice.
81. 85 Ambula. (n.d.). What Are the Best Orthopedics Marketing Strategies?
82. 86 SocialClimb. (n.d.). Strategies for Expanding Your Orthopedic Practice.
83. 87 RRY Publications LLC. (n.d.). Business of Orthopedics.
84. 88 The OrthoForum. (n.d.). 3 Big Challenges for Growing Orthopaedic Practices.
85. 89 Elexes. (n.d.). Challenges for Medical Device Manufacturers.
86. 56 Vantage Medtech. (n.d.). Top Challenges For Medical Device Manufacturers (And How to Overcome Them).
87. 90 BONEZONE. (2022). Orthopedic Market Experiences Familiar Challenges in Push Toward Recovery.
88. 91 MedWorld Advisors. (2025). Juggling the Orthopedic Manufacturing Challenges of 2025: Nearshoring, M&A, and Tariffs.
89. 57 ImplantBase. (n.d.). Field Inventory Management for Orthopedic Medical Device Companies: Challenges and Solutions.
90. 46 ClickUp. (n.d.). How to Start an Orthopedic Device Manufacturing Business.
91. 92 University Lab Partners. (n.d.). Navigating Regulatory Pathways: Implications for Medical Device Startups.
92. 93 Isaacson, B., et al. (2022). Translational success in medical devices: a case study of collaboration and cooperation.
Journal of Translational Medicine, 20(1), 127.
93. 94 Greenlight Guru. (n.d.). Bringing a Medical Device to Market: A Step-by-Step Guide.
94. 95 Knobbe Martens. (n.d.). Medical Device Innovations and IP Strategy.
95. 96 Menicucci, G., et al. (2025). The Impact of Insertion Torque on Bone Stress around Ultra-Short Dental Implants: A Finite Element Analysis.
Journal of Functional Biomaterials, 16(7), 260.
96. 97 Romero, M., et al. (2025). The Topography of Titanium in Dental Implants: Key to Osseointegration and Bactericidal Capacity.
Materials, 18(14), 3368.
97. 5 Wikipedia. (n.d.). Osseointegration.
98. 98 Various Authors. (n.d.). Osseointegration Publications.
ResearchGate.
99. 60 Gupta, S., et al. (2022). Contemporary Concepts in Osseointegration of Dental Implants: A Review.
BioMed Research International, 2022, 6170452.
100. 6 Albrektsson, T., & Zarb, G. (1985). Osseointegration: A review.
Quintessence International, 16(1), 35-41.
101. 61 RAPS. (2024). FDA proposes guidance on orthopedic product coatings.
102. 62 U.S. Food and Drug Administration. (1995). 510(k) Information Needed for Hydroxyapatite Coated Orthopedic Implants.